You Have Got Fallen Arches?
Overview
The most common arch problem is the flat foot. This sometimes starts in childhood or may gradually develop in adulthood. In most cases the flat foot is related to a tight calf. The tightness of the calf forces the foot to overpronate (the inside of the foot rolls inwards) and the arch to break down and collapse. The arch collapse leads to abnormal stress on the plantar fascia leading to heel pain, as well as to the main medial tendon (the posterior tibial tendon), leading to tendonitis and even tears of the tendon. The other common symptom in severe flat feet is pain on the outside of the foot as well as calf and Achilles symptoms.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Feet tire easily and become painful and achy, especially around the arch, ankle and heel. Swelling on the inside bottom of your feet. Back and leg pain. Difficulty standing on toes.
Diagnosis
Diagnosis of flat feet or fallen arches can be made by your health practitioner and is based on the following. Clinical assessment involving visual gait assessment, as well as biomechanical assessment. A detailed family and medical history. A pain history assessment determining the location of painful symptoms. Physical palpation of the feet and painful areas. Imaging such as MRI or x-ray can be used by your practitioner to assist in the diagnosis.
fallen arches support
Non Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Surgical Treatment

Common indications for surgery are cerebral palsy with an equinovalgus foot, to prevent progression and breakdown of the midfoot. Rigid and painful Pes Planus. To prevent progression, eg with a Charcot joint. Tibialis posterior dysfunction, where non-surgical treatment is unsuccessful. Possible surgical procedures include Achilles tendon lengthening. Calcaneal osteotomy, to re-align the hindfoot. Reconstruction of the tibialis posterior tendon. For severe midfoot collapse of the arch, triple arthrodesis may be indicated.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
The most common arch problem is the flat foot. This sometimes starts in childhood or may gradually develop in adulthood. In most cases the flat foot is related to a tight calf. The tightness of the calf forces the foot to overpronate (the inside of the foot rolls inwards) and the arch to break down and collapse. The arch collapse leads to abnormal stress on the plantar fascia leading to heel pain, as well as to the main medial tendon (the posterior tibial tendon), leading to tendonitis and even tears of the tendon. The other common symptom in severe flat feet is pain on the outside of the foot as well as calf and Achilles symptoms.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Feet tire easily and become painful and achy, especially around the arch, ankle and heel. Swelling on the inside bottom of your feet. Back and leg pain. Difficulty standing on toes.
Diagnosis
Diagnosis of flat feet or fallen arches can be made by your health practitioner and is based on the following. Clinical assessment involving visual gait assessment, as well as biomechanical assessment. A detailed family and medical history. A pain history assessment determining the location of painful symptoms. Physical palpation of the feet and painful areas. Imaging such as MRI or x-ray can be used by your practitioner to assist in the diagnosis.
fallen arches support
Non Surgical Treatment
In rare cases, surgery may be needed if a child has flat feet caused by a problem they're born with (a congenital abnormality). The foot may need to be straightened or the bones may need to be separated if they're fused together. Painkillers and insoles are the first treatment options for flat feet that are caused by a joint problem, such as arthritis or a torn tendon. However, surgery may be recommended if the injury or condition is severely affecting your feet. Where flat feet are caused by a condition that affects the nervous system, special shoes, insoles, or supportive foot or leg braces may be needed. Again, in severe cases, an operation may be needed to straighten the feet.
Surgical Treatment

Common indications for surgery are cerebral palsy with an equinovalgus foot, to prevent progression and breakdown of the midfoot. Rigid and painful Pes Planus. To prevent progression, eg with a Charcot joint. Tibialis posterior dysfunction, where non-surgical treatment is unsuccessful. Possible surgical procedures include Achilles tendon lengthening. Calcaneal osteotomy, to re-align the hindfoot. Reconstruction of the tibialis posterior tendon. For severe midfoot collapse of the arch, triple arthrodesis may be indicated.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Apparent Leg Length Discrepancy Therapy
Overview
Small or mild length leg discrepancies (LLD), i.e., below 3.0 cm, have been considered as enough to cause orthopaedic changes such as lumbar pain, stress fractures and osteoarthritis on lower limbs (LLLL) joints. In addition to the classification by its magnitude, discrepancies can also be categorized according to etiology, being structural when a difference is noted between bone structures' length or functional as a result of mechanical changes on the lower limb, and are found in 65% - 70% of the healthy population.
Causes
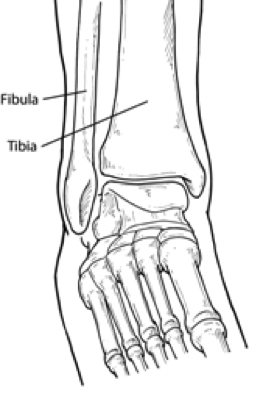
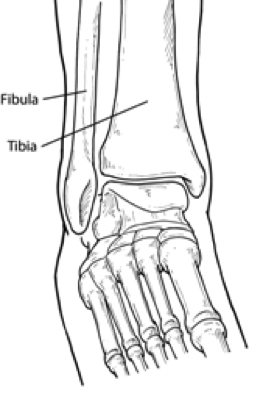
The causes of LLD may be divided into those that shorten a limb versus those that lengthen a limb, or they may be classified as affecting the length versus the rate of growth in a limb. For example, a fracture that heals poorly may shorten a leg slightly, but does not affect its growth rate. Radiation, on the other hand, can affect a leg's long-term ability to expand, but does not acutely affect its length. Causes that shorten the leg are more common than those that lengthen it and include congenital growth deficiencies (seen in hemiatrophy and skeletal dysplasias ), infections that infiltrate the epiphysis (e.g. osteomyelitis ), tumors, fractures that occur through the growth plate or have overriding ends, Legg-Calve-Perthes disease, slipped capital femoral epiphysis (SCFE), and radiation. Lengthening can result from unique conditions, such as hemihypertrophy , in which one or more structures on one side of the body become larger than the other side, vascular malformations or tumors (such as hemangioma ), which cause blood flow on one side to exceed that of the other, Wilm's tumor (of the kidney), septic arthritis, healed fractures, or orthopaedic surgery. Leg length discrepancy may arise from a problem in almost any portion of the femur or tibia. For example, fractures can occur at virtually all levels of the two bones. Fractures or other problems of the fibula do not lead to LLD, as long as the more central, weight-bearing tibia is unaffected. Because many cases of LLD are due to decreased rate of growth, the femoral or tibial epiphyses are commonly affected regions.
Symptoms
Often there are few or no symptoms prior to the age of 25-35. The most common symptom is chronic lower back pain, but also is frequently middle and upper back pain. Same-sided and repeated injury or pain to the hip, knee and/or ankle is also a hallmark of a long-standing untreated LLD. It is not uncommon to have buttock or radiating hip pain that is non-dermatomal (not from a disc) and tends to go away when lying down.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.

functional leg length discrepancy treatment
Surgical Treatment
Surgical lengthening of the shorter extremity (upper or lower) is another treatment option. The bone is lengthened by surgically applying an external fixator to the extremity in the operating room. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins or both. A small crack is made in the bone and tension is created by the frame when it is "distracted" by the patient or family member who turns an affixed dial several times daily. The lengthening process begins approximately five to ten days after surgery. The bone may lengthen one millimeter per day, or approximately one inch per month. Lengthening may be slower in adults overall and in a bone that has been previously injured or undergone prior surgery. Bones in patients with potential blood vessel abnormalities (i.e., cigarette smokers) may also lengthen more slowly. The external fixator is worn until the bone is strong enough to support the patient safely, approximately three months per inch of lengthening. This may vary, however, due to factors such as age, health, smoking, participation in rehabilitation, etc. Risks of this procedure include infection at the site of wires and pins, stiffness of the adjacent joints and slight over or under correction of the bone?s length. Lengthening requires regular follow up visits to the physician?s office, meticulous hygiene of the pins and wires, diligent adjustment of the frame several times daily and rehabilitation as prescribed by your physician.
Small or mild length leg discrepancies (LLD), i.e., below 3.0 cm, have been considered as enough to cause orthopaedic changes such as lumbar pain, stress fractures and osteoarthritis on lower limbs (LLLL) joints. In addition to the classification by its magnitude, discrepancies can also be categorized according to etiology, being structural when a difference is noted between bone structures' length or functional as a result of mechanical changes on the lower limb, and are found in 65% - 70% of the healthy population.

Causes
The causes of LLD may be divided into those that shorten a limb versus those that lengthen a limb, or they may be classified as affecting the length versus the rate of growth in a limb. For example, a fracture that heals poorly may shorten a leg slightly, but does not affect its growth rate. Radiation, on the other hand, can affect a leg's long-term ability to expand, but does not acutely affect its length. Causes that shorten the leg are more common than those that lengthen it and include congenital growth deficiencies (seen in hemiatrophy and skeletal dysplasias ), infections that infiltrate the epiphysis (e.g. osteomyelitis ), tumors, fractures that occur through the growth plate or have overriding ends, Legg-Calve-Perthes disease, slipped capital femoral epiphysis (SCFE), and radiation. Lengthening can result from unique conditions, such as hemihypertrophy , in which one or more structures on one side of the body become larger than the other side, vascular malformations or tumors (such as hemangioma ), which cause blood flow on one side to exceed that of the other, Wilm's tumor (of the kidney), septic arthritis, healed fractures, or orthopaedic surgery. Leg length discrepancy may arise from a problem in almost any portion of the femur or tibia. For example, fractures can occur at virtually all levels of the two bones. Fractures or other problems of the fibula do not lead to LLD, as long as the more central, weight-bearing tibia is unaffected. Because many cases of LLD are due to decreased rate of growth, the femoral or tibial epiphyses are commonly affected regions.
Symptoms
Often there are few or no symptoms prior to the age of 25-35. The most common symptom is chronic lower back pain, but also is frequently middle and upper back pain. Same-sided and repeated injury or pain to the hip, knee and/or ankle is also a hallmark of a long-standing untreated LLD. It is not uncommon to have buttock or radiating hip pain that is non-dermatomal (not from a disc) and tends to go away when lying down.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.

functional leg length discrepancy treatment
Surgical Treatment
Surgical lengthening of the shorter extremity (upper or lower) is another treatment option. The bone is lengthened by surgically applying an external fixator to the extremity in the operating room. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins or both. A small crack is made in the bone and tension is created by the frame when it is "distracted" by the patient or family member who turns an affixed dial several times daily. The lengthening process begins approximately five to ten days after surgery. The bone may lengthen one millimeter per day, or approximately one inch per month. Lengthening may be slower in adults overall and in a bone that has been previously injured or undergone prior surgery. Bones in patients with potential blood vessel abnormalities (i.e., cigarette smokers) may also lengthen more slowly. The external fixator is worn until the bone is strong enough to support the patient safely, approximately three months per inch of lengthening. This may vary, however, due to factors such as age, health, smoking, participation in rehabilitation, etc. Risks of this procedure include infection at the site of wires and pins, stiffness of the adjacent joints and slight over or under correction of the bone?s length. Lengthening requires regular follow up visits to the physician?s office, meticulous hygiene of the pins and wires, diligent adjustment of the frame several times daily and rehabilitation as prescribed by your physician.
Heel Soreness All You Might Want To Understand Heel Discomfort
Overview

The most common form of heel pain, is pain on the bottom of the heel. It tends to occur for no apparent reason and is often worse when first placing weight on the foot. Patients often complain of pain the first thing in the morning or after getting up to stand after sitting. The pain can be a sharp, searing pain or present as a tearing feeling in the bottom of the heel. As the condition progresses there may be a throbbing pain after getting off your feet or there may be soreness that radiates up the back of the leg. Pain may also radiate into the arch of the foot.
Causes
Plantar fasciitis is caused by inflammation and irritation of the tight tissue forming the arch of the foot. The most common cause of heel pain, it typically affects men, aged 40 - 70 who are physically active. The bottom or inside of the foot and / or heel (where heel and arch meet) may hurt or cause severe pain upon standing after resting -- or most often, when arising in the morning. The pain is usually experienced within the first few steps and is often characterized as "walking on nails" or knife blades. The pain may let up after walking a bit but most commonly returns after prolonged movement or a rest.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heelsncleavage
Prevention

Maintaining flexible and strong muscles in your calves, ankles, and feet can help prevent some types of heel pain. Always stretch and warm-up before exercising. Wear comfortable, properly fitting shoes with good arch support and cushioning. Make sure there is enough room for your toes.

The most common form of heel pain, is pain on the bottom of the heel. It tends to occur for no apparent reason and is often worse when first placing weight on the foot. Patients often complain of pain the first thing in the morning or after getting up to stand after sitting. The pain can be a sharp, searing pain or present as a tearing feeling in the bottom of the heel. As the condition progresses there may be a throbbing pain after getting off your feet or there may be soreness that radiates up the back of the leg. Pain may also radiate into the arch of the foot.
Causes
Plantar fasciitis is caused by inflammation and irritation of the tight tissue forming the arch of the foot. The most common cause of heel pain, it typically affects men, aged 40 - 70 who are physically active. The bottom or inside of the foot and / or heel (where heel and arch meet) may hurt or cause severe pain upon standing after resting -- or most often, when arising in the morning. The pain is usually experienced within the first few steps and is often characterized as "walking on nails" or knife blades. The pain may let up after walking a bit but most commonly returns after prolonged movement or a rest.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Most patients get better with the help of nonsurgical treatments. Stretches for the calf muscles on the back of the lower leg take tension off the plantar fascia. A night splint can be worn while you sleep. The night splint keeps your foot from bending downward. It places a mild stretch on the calf muscles and the plantar fascia. Some people seem to get better faster when using a night splint. They report having less heel pain when placing the sore foot on the ground in the morning. There have been a few studies that reported no significant benefit from adding night splinting to a program of antiinflammatory meds and stretching. Other studies report the benefits of short-term casting to unload the heel, immobilize the plantar fascia, and reduce repetitive microtrauma. Supporting the arch with a well fitted arch support, or orthotic, may also help reduce pressure on the plantar fascia. Placing a special type of insert into the shoe, called a heel cup, can reduce the pressure on the sore area. Wearing a silicone heel pad adds cushion to a heel that has lost some of the fat pad through degeneration. Shock wave therapy is a newer form of nonsurgical treatment. It uses a machine to generate shock wave pulses to the sore area. Patients generally receive the treatment once each week for up to three weeks. It is not known exactly why it works for plantar fasciitis. It's possible that the shock waves disrupt the plantar fascial tissue enough to start a healing response. The resulting release of local growth factors and stem cells causes an increase in blood flow to the area. Recent studies indicate that this form of treatment can help ease pain, while improving range of motion and function.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heelsncleavage
Prevention

Maintaining flexible and strong muscles in your calves, ankles, and feet can help prevent some types of heel pain. Always stretch and warm-up before exercising. Wear comfortable, properly fitting shoes with good arch support and cushioning. Make sure there is enough room for your toes.
Mortons Neuroma Remedies
Overview
 Morton's metatarsalgia is a condition associated with a painful neuroma* on the digital nerve causing pain in the foot. Charcterised by perineural fibrosis and nerve degeneration due to repetitive irritation, is thought to be due to irritation of the digital nerve caused by repeated trauma, ischemia or entrapment of the nerve, occurs most frequently in women aged 40-50 who wear high-heeled, pointed-toe shoes. The neuroma occurs at the level of the metatarsal necks. The common digital nerve to the third/fourth metatarsal spaces is most often affected, although other interspaces can be involved.
Morton's metatarsalgia is a condition associated with a painful neuroma* on the digital nerve causing pain in the foot. Charcterised by perineural fibrosis and nerve degeneration due to repetitive irritation, is thought to be due to irritation of the digital nerve caused by repeated trauma, ischemia or entrapment of the nerve, occurs most frequently in women aged 40-50 who wear high-heeled, pointed-toe shoes. The neuroma occurs at the level of the metatarsal necks. The common digital nerve to the third/fourth metatarsal spaces is most often affected, although other interspaces can be involved.
Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Morton?s neuroma is a progressive condition which means the symptoms typically get worse over time. Initially people often complain of a tingling or numbness at the base of their toes, typically in the space between the third and fourth toes, or, less commonly , between the second and third toes, which feels a bit like pins and needles. Over time the pain progresses and can feel like a stabbing or burning sensation in the ball of the foot under the toes. Some describe it as feeling as if they are standing on a stone. Normally the pain will get worse when you wear tight fitting shoes. Doing exercise that impacts on the foot such as jogging can also make the symptoms worse. The extent of the pain varies from person to person but in some cases it can be so intense that every step can feel acutely painful.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
There are various options for treating the condition, depending on its severity. Self-treatment. Here are some simple steps that may improve symptoms. Wear supportive shoes with a wide toe box. Do not lace the forefoot of the shoe too tightly. Shoes with shock-absorbent soles and proper insoles are recommended. Do not wear tight or pointed toed shoes or shoes with heels more than 2 inches high. Use over-the-counter shoe pads to relieve pressure. Apply an ice pack to the affected area to reduce pain and swelling. Rest your feet and massage the painful area. There are drugs that may temporarily relieve the pain and other symptoms of Morton?s neuroma. Long-term use of these medications is not recommended. Anti-inflammatory drugs-Nonsteroidal anti-inflammatory drugs, such as ibuprofen or aspirin, may be taken orally to reduce pain and inflammation. Anti-inflammatory drugs can also be administered by direct injection into the skin. Local anesthetic. An anesthetic injection will temporarily relieve pain by numbing the affected nerve. Orthotics. These are custom-designed shoe inserts that can reduce some of the pain associated with Morton?s neuroma. Sometimes padding is placed around the toe area, and tape is applied to hold the padding in place.
Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
 Morton's metatarsalgia is a condition associated with a painful neuroma* on the digital nerve causing pain in the foot. Charcterised by perineural fibrosis and nerve degeneration due to repetitive irritation, is thought to be due to irritation of the digital nerve caused by repeated trauma, ischemia or entrapment of the nerve, occurs most frequently in women aged 40-50 who wear high-heeled, pointed-toe shoes. The neuroma occurs at the level of the metatarsal necks. The common digital nerve to the third/fourth metatarsal spaces is most often affected, although other interspaces can be involved.
Morton's metatarsalgia is a condition associated with a painful neuroma* on the digital nerve causing pain in the foot. Charcterised by perineural fibrosis and nerve degeneration due to repetitive irritation, is thought to be due to irritation of the digital nerve caused by repeated trauma, ischemia or entrapment of the nerve, occurs most frequently in women aged 40-50 who wear high-heeled, pointed-toe shoes. The neuroma occurs at the level of the metatarsal necks. The common digital nerve to the third/fourth metatarsal spaces is most often affected, although other interspaces can be involved.Causes
Anything that causes compression or irritation of the nerve can lead to the development of a neuroma. One of the most common causes comes from wearing shoes that have a tapered toe box, or high-heeled shoes that cause the toes to be forced into the toe box and overload pressure onto the forefoot. An injury or trauma to the forefoot may also lead to a neuroma. People at a higher risk of developing a Neuroma include people with certain foot deformities, such as bunions or hammertoes. Certain foot types, such as flat feet (Pronation) More flexible feet, and woman after pregnancy.
Symptoms
Morton?s neuroma is a progressive condition which means the symptoms typically get worse over time. Initially people often complain of a tingling or numbness at the base of their toes, typically in the space between the third and fourth toes, or, less commonly , between the second and third toes, which feels a bit like pins and needles. Over time the pain progresses and can feel like a stabbing or burning sensation in the ball of the foot under the toes. Some describe it as feeling as if they are standing on a stone. Normally the pain will get worse when you wear tight fitting shoes. Doing exercise that impacts on the foot such as jogging can also make the symptoms worse. The extent of the pain varies from person to person but in some cases it can be so intense that every step can feel acutely painful.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
There are various options for treating the condition, depending on its severity. Self-treatment. Here are some simple steps that may improve symptoms. Wear supportive shoes with a wide toe box. Do not lace the forefoot of the shoe too tightly. Shoes with shock-absorbent soles and proper insoles are recommended. Do not wear tight or pointed toed shoes or shoes with heels more than 2 inches high. Use over-the-counter shoe pads to relieve pressure. Apply an ice pack to the affected area to reduce pain and swelling. Rest your feet and massage the painful area. There are drugs that may temporarily relieve the pain and other symptoms of Morton?s neuroma. Long-term use of these medications is not recommended. Anti-inflammatory drugs-Nonsteroidal anti-inflammatory drugs, such as ibuprofen or aspirin, may be taken orally to reduce pain and inflammation. Anti-inflammatory drugs can also be administered by direct injection into the skin. Local anesthetic. An anesthetic injection will temporarily relieve pain by numbing the affected nerve. Orthotics. These are custom-designed shoe inserts that can reduce some of the pain associated with Morton?s neuroma. Sometimes padding is placed around the toe area, and tape is applied to hold the padding in place.

Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
Recovery Time After Accessory Navicular Surgery
Overview
An accessory navicular is defined as an extra bone in the foot, and oftentimes it causes moderate to severe discomfort. Depending on the severity, your doctor may recommend a non-surgical treatment to alleviate the pain, or surgery if treatment doesn?t decrease symptoms.
Causes
It is commonly believed that the posterior tibial tendon loses its vector of pull to heighten the arch. As the posterior muscle contracts, the tendon is no longer pulling straight up on the navicular but must course around the prominence of bone and first pull medially before pulling upward. In addition, the enlarged bones may irritate and damage the insertional area of the posterior tibial tendon, making it less functional. Therefore, the presence of the accessory navicular bone does contribute to posterior tibial dysfunction.
Symptoms
The main symptom of an aggravated accessory navicular is pain, particularly in the instep. Walking can sometimes be difficult, and tight shoes may worsen the condition.
Diagnosis
Typically, accessory navicular syndrome isn?t hard to diagnose. Our podiatrists will examine the lower limb and check the hard prominence, as well as use X-rays to confirm the presence of extra bone tissue. Other diagnostic images may be able to identify inflammation and specific damage to the midfoot. Depending on the severity of your discomfort, conservative measures may be enough to resolve the condition.
Non Surgical Treatment
Treating accessory navicular syndrome is focused on relieving symptoms. Some treatment methods are Icing to reduce swelling. Immobilization with a cast or walking boot to reduce inflammation and promote healing. Medications to reduce pain and inflammation. Physical therapy to strengthen muscles. Orthotics to support the arch. Surgery may be needed to remove the accessory bone and reshape the area if other methods are not successful.

Surgical Treatment
Surgery may be an option if non-surgical treatment does not decrease the symptoms of accessory navicular syndrome. Since this bone is not needed for the foot to function normally, Your surgeon may remove the accessory navicular, reshape the area, and repair the posterior tibial tendon for improved function.
An accessory navicular is defined as an extra bone in the foot, and oftentimes it causes moderate to severe discomfort. Depending on the severity, your doctor may recommend a non-surgical treatment to alleviate the pain, or surgery if treatment doesn?t decrease symptoms.
Causes
It is commonly believed that the posterior tibial tendon loses its vector of pull to heighten the arch. As the posterior muscle contracts, the tendon is no longer pulling straight up on the navicular but must course around the prominence of bone and first pull medially before pulling upward. In addition, the enlarged bones may irritate and damage the insertional area of the posterior tibial tendon, making it less functional. Therefore, the presence of the accessory navicular bone does contribute to posterior tibial dysfunction.
Symptoms
The main symptom of an aggravated accessory navicular is pain, particularly in the instep. Walking can sometimes be difficult, and tight shoes may worsen the condition.
Diagnosis
Typically, accessory navicular syndrome isn?t hard to diagnose. Our podiatrists will examine the lower limb and check the hard prominence, as well as use X-rays to confirm the presence of extra bone tissue. Other diagnostic images may be able to identify inflammation and specific damage to the midfoot. Depending on the severity of your discomfort, conservative measures may be enough to resolve the condition.
Non Surgical Treatment
Treating accessory navicular syndrome is focused on relieving symptoms. Some treatment methods are Icing to reduce swelling. Immobilization with a cast or walking boot to reduce inflammation and promote healing. Medications to reduce pain and inflammation. Physical therapy to strengthen muscles. Orthotics to support the arch. Surgery may be needed to remove the accessory bone and reshape the area if other methods are not successful.

Surgical Treatment
Surgery may be an option if non-surgical treatment does not decrease the symptoms of accessory navicular syndrome. Since this bone is not needed for the foot to function normally, Your surgeon may remove the accessory navicular, reshape the area, and repair the posterior tibial tendon for improved function.
Exercises To Help Accessory Navicular Syndrome
Overview
Accessory navicular syndrome is the painful condition caused by the presence of the accessory navicular. Well, is the statement a bit confusing? Let me explain. The accessory navicular is a bone in the foot that is not supposed to be present. But in some very rare cases, this extra bone (sometimes can also be a cartilage piece) is present by birth. This bone exists in the arch of the foot. The presence of this bone though not common, is not abnormal either as most people are not even aware of its existence unless and until it begins to cause pain which we call accessory navicular syndrome.

Causes
An accessory navicular develops as a result of a congenital anomaly and is found more often in women. If the bone is large, it may rub against a shoe, causing pain. Because of its location, the posterior tibial tendon may pull on the bone during walking or running, causing the fibrous tissue that connects the accessory navicular to the navicular to tear and become inflamed.
Symptoms
The symptoms of accessory navicular syndrome commonly arise during adolescence, when bones are maturing and cartilage fuses into bone. In other instances, symptoms do not appAccessory Navicularear until adulthood. The signs and symptoms include a visible bony prominence on the midfoot the inner side of the foot above the arch. Redness or swelling of the bony prominence. Indistinct pain or throbbing in the midfoot and arch during or after physical activity.
Diagnosis
Diagnosis starts by speaking with the patient about symptoms. The physician will look at the foot and examine it for signs of an accessory navicular. By putting pressure on the area, the doctor may determine its presence simply by the presence of pain. The muscle, joint, and the overall structure of the foot may be considered, as well as the way in which the patient walks. If a diagnosis of accessory navicular syndrome is made, an X-ray or MRI may be ordered to confirm diagnosis.
Non Surgical Treatment
Fortunately, surgery is not the only answer when it comes to relieving symptoms of accessory navicular syndrome. The physician may recommend wearing a cast or walking boot for a period of time so the foot can recover from the inflammation. Ice may be used to relieve swelling, too, although it should be wrapped to avoid direct contact with the skin.

Surgical Treatment
The Kidner procedure involves resecting the prominent accessory navicular and ensuring that the posterior tibial tendon is still attached to the bone. Often the prominent bone can simply be shelled out from its position relative to the posterior tibial tendon, which leaves the tendon intact. However, if the tendon is loose and floppy once the extra bone has been removed, suturing or tother is required as a means of attaching it into the remaining navicular bone.
Accessory navicular syndrome is the painful condition caused by the presence of the accessory navicular. Well, is the statement a bit confusing? Let me explain. The accessory navicular is a bone in the foot that is not supposed to be present. But in some very rare cases, this extra bone (sometimes can also be a cartilage piece) is present by birth. This bone exists in the arch of the foot. The presence of this bone though not common, is not abnormal either as most people are not even aware of its existence unless and until it begins to cause pain which we call accessory navicular syndrome.

Causes
An accessory navicular develops as a result of a congenital anomaly and is found more often in women. If the bone is large, it may rub against a shoe, causing pain. Because of its location, the posterior tibial tendon may pull on the bone during walking or running, causing the fibrous tissue that connects the accessory navicular to the navicular to tear and become inflamed.
Symptoms
The symptoms of accessory navicular syndrome commonly arise during adolescence, when bones are maturing and cartilage fuses into bone. In other instances, symptoms do not appAccessory Navicularear until adulthood. The signs and symptoms include a visible bony prominence on the midfoot the inner side of the foot above the arch. Redness or swelling of the bony prominence. Indistinct pain or throbbing in the midfoot and arch during or after physical activity.
Diagnosis
Diagnosis starts by speaking with the patient about symptoms. The physician will look at the foot and examine it for signs of an accessory navicular. By putting pressure on the area, the doctor may determine its presence simply by the presence of pain. The muscle, joint, and the overall structure of the foot may be considered, as well as the way in which the patient walks. If a diagnosis of accessory navicular syndrome is made, an X-ray or MRI may be ordered to confirm diagnosis.
Non Surgical Treatment
Fortunately, surgery is not the only answer when it comes to relieving symptoms of accessory navicular syndrome. The physician may recommend wearing a cast or walking boot for a period of time so the foot can recover from the inflammation. Ice may be used to relieve swelling, too, although it should be wrapped to avoid direct contact with the skin.

Surgical Treatment
The Kidner procedure involves resecting the prominent accessory navicular and ensuring that the posterior tibial tendon is still attached to the bone. Often the prominent bone can simply be shelled out from its position relative to the posterior tibial tendon, which leaves the tendon intact. However, if the tendon is loose and floppy once the extra bone has been removed, suturing or tother is required as a means of attaching it into the remaining navicular bone.
Shoe Lifts For Leg Length Discrepancy
There are not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter in comparison to the other. Through developmental periods of aging, the human brain senses the gait pattern and identifies some variation. The entire body typically adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch isn't very irregular, require Shoe Lifts to compensate and normally doesn't have a profound effect over a lifetime.

Leg length inequality goes typically undiagnosed on a daily basis, yet this issue is very easily solved, and can reduce numerous cases of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts . These are typically affordable, commonly being below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is easily the most prevalent condition affecting people today. Around 80 million men and women experience back pain at some stage in their life. It's a problem which costs employers millions of dollars annually on account of time lost and output. Innovative and improved treatment solutions are continually sought after in the hope of decreasing the economic impact this condition causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In most of these cases Shoe Lifts might be of worthwhile. The lifts are capable of eliminating any discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
So as to support the human body in a nicely balanced manner, feet have got a critical job to play. Irrespective of that, it is sometimes the most overlooked region of the human body. Some people have flat-feet which means there may be unequal force placed on the feet. This will cause other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts make sure that ideal posture and balance are restored.

Leg length inequality goes typically undiagnosed on a daily basis, yet this issue is very easily solved, and can reduce numerous cases of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts . These are typically affordable, commonly being below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Low back pain is easily the most prevalent condition affecting people today. Around 80 million men and women experience back pain at some stage in their life. It's a problem which costs employers millions of dollars annually on account of time lost and output. Innovative and improved treatment solutions are continually sought after in the hope of decreasing the economic impact this condition causes.

People from all corners of the earth suffer the pain of foot ache as a result of leg length discrepancy. In most of these cases Shoe Lifts might be of worthwhile. The lifts are capable of eliminating any discomfort in the feet. Shoe Lifts are recommended by many certified orthopaedic practitioners".
So as to support the human body in a nicely balanced manner, feet have got a critical job to play. Irrespective of that, it is sometimes the most overlooked region of the human body. Some people have flat-feet which means there may be unequal force placed on the feet. This will cause other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts make sure that ideal posture and balance are restored.